The nervous system—comprising the brain, spinal cord, and all associated nerves—is the master control center of the human body. In children, this system is not static; it is rapidly and profoundly developing. When an illness, injury, or genetic factor disrupts this process, the result is a pediatric neurological disorder.
These conditions are unique because they interfere with critical developmental milestones, potentially affecting a child’s movement, speech, learning, and social interaction. For parents and caregivers, recognizing the early and often subtle signs of these disorders is crucial, as the intervention provided during early childhood can dramatically alter a child’s developmental trajectory.
In a specialized practice like that of Dr. Habib G Pathan, Senior Consultant Pediatric Neurologist and Director of Dr. Habib’s Foster CDC the philosophy is clear: Early Intervention is Key for early brain development. This comprehensive guide details the major categories of child neurological disorders and their associated symptoms, underscoring the necessity of seeking specialized care promptly.
Neurodevelopmental Disorders: Challenges in Learning and Behavior
This vast category includes conditions that begin early in development, characterized by persistent developmental deficits that affect personal, social, academic, or occupational functioning. These disorders often require a multidisciplinary team approach involving neurologists, psychologists, and specialized therapists.
- Autism Spectrum Disorder (ASD)
Autism Spectrum Disorder (ASD) is a developmental condition affecting social communication, interaction, and behavior. It is defined by a spectrum because its severity and presentation vary widely.
Core Symptoms in Children:
- Deficits in Social Communication and Interaction:
- Impaired Nonverbal Cues: Failure to consistently use or understand eye contact, facial expressions, and body language to regulate social interaction.
- Social Reciprocity: Lack of “back-and-forth” conversation, limited sharing of interests, or difficulty initiating or maintaining conversations relevant to others’ interests.
- Relationship Challenges: Difficulty making friends, limited imaginative play with peers, or seeming unaware of others’ feelings.
- Restricted, Repetitive Patterns of Behavior, Interests, or Activities (RRBs):
- Stereotyped Movements: Repetitive motor mannerisms such as hand flapping, toe-walking, spinning, or rocking.
- Insistence on Sameness: Rigid adherence to specific, non-functional routines; extreme distress or meltdowns following small changes in the environment or schedule.
- Highly Restricted Interests: Intense preoccupation with specific topics (e.g., trains, vacuums, video game stats) that is abnormal in focus or intensity.
- Sensory Sensitivities: Hyper- (overly sensitive) or hypo- (underly sensitive) reactions to sensory input, such as adverse reactions to loud noises, certain textures, or an unusual fascination with lights or movement.
Treatment Focus: Early and intensive behavioral and communication therapies (like ABA, Speech Therapy) are critical.
- Attention-Deficit/Hyperactivity Disorder (ADHD)
Attention-Deficit/Hyperactivity Disorder (ADHD) is a neurodevelopmental condition marked by persistent patterns of inattention and/or hyperactivity-impulsivity that severely interfere with functioning. As highlighted by Dr. Habib’s clinic, it is a frequent focus of neurobehavioral intervention.
Symptoms by Presentation:
- Inattentive Presentation:
- Easily distracted by stimuli unrelated to the task at hand.
- Difficulty sustaining attention in play, tasks, or conversations.
- Trouble following through on instructions, often failing to complete homework or chores.
- Often disorganized, frequently losing necessary items (books, keys, tools).
- Appears not to listen when spoken to directly.
- Hyperactive-Impulsive Presentation:
- Excessive fidgeting, tapping hands, or squirming in the seat.
- Difficulty engaging in quiet play or activities.
- Excessive talking and blurting out answers before questions are finished (impulsivity).
- Trouble waiting for their turn in games or lines.
- Running or climbing in situations where it is inappropriate.
Treatment Focus: A multimodal approach combining medication (stimulants or non-stimulants) and behavioral therapy, including parent management training and educational interventions.
- Developmental Delays and Learning Disabilities
Developmental Delay (DD) is often the earliest red flag, indicating a child is not meeting expected milestones. When the delay affects two or more developmental areas in children under age five, it is termed Global Developmental Delay (GDD).
- Symptoms of DD: Late acquisition of walking, talking, grasping small objects, or demonstrating poor social skills relative to peers.
- Specific Learning Disabilities (SLD): These are neurological disorders that affect the brain’s ability to receive, process, analyze, or store information.
- Dyslexia: Difficulty with reading and accurate word recognition (phonological processing).
- Dysgraphia: Difficulty with writing, spelling, and organizing thoughts on paper.
- Dyscalculia: Difficulty performing mathematical calculations and understanding number sense.
Treatment Focus: Targeted therapies (Speech, Occupational, Remedial Education) that address the specific area of delay or disability.
- Motor and Movement Disorders: The Control Center Disrupted
These disorders involve damage to the motor control centers of the brain or progressive disease in the muscles themselves, leading to issues with muscle tone, posture, and coordination.
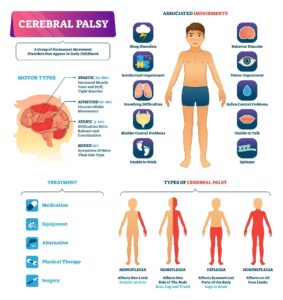
- Cerebral Palsy (CP)
Cerebral Palsy (CP) is the most common motor disability of childhood. It is a non-progressive condition resulting from damage to the developing brain, often occurring before or around the time of birth (e.g., from hypoxia, infection, or hemorrhage).
Symptoms and Types:
CP is classified by the type of movement problem and the part of the body affected.
- Spastic CP (Most Common): Characterized by high muscle tone (hypertonia or spasticity), making movements stiff and exaggerated. This is caused by damage to the brain’s motor cortex.
- Spastic Diplegia: Stiffness predominantly in the legs, often causing a “scissor gait.”
- Spastic Hemiplegia: Affects one side of the body (e.g., one arm and one leg).
- Spastic Quadriplegia: Affects all four limbs and the trunk, often associated with the most severe developmental challenges.
- Dyskinetic CP: Characterized by uncontrollable, slow, and often writhing movements (athetosis or dystonia), resulting from damage to the basal ganglia.
- Symptoms: Involuntary movements that interfere with speech, feeding, and voluntary actions.
- Ataxic CP: Characterized by poor coordination, poor balance, and shakiness (tremor), resulting from damage to the cerebellum.
Early Symptoms: Delayed motor milestones (late to roll, sit, or walk), unusual muscle tone (too stiff or too floppy), or reliance on only one side of the body.
- Neuromuscular and Muscle Disorders
These conditions affect the nerves that control voluntary muscles or the muscles themselves. Dr. Habib’s practice treats muscle disorders such as hypotonia, dystonia, and muscular dystrophies.
- Muscular Dystrophy (MD): A group of inherited genetic disorders causing progressive muscle weakness and loss of muscle mass.
- Duchenne Muscular Dystrophy (DMD): The most severe and common type. Symptoms appear early (age 2-3) and include frequent falling, difficulty running, and using hands to “walk” up the legs to stand
- Hypotonia (Floppy Baby Syndrome): Abnormally low muscle tone, often present at birth. While a symptom of many underlying conditions (like CP, genetic syndromes, or peripheral nerve disorders), it requires immediate neurological evaluation.
Treatment Focus: Physical therapy, occupational therapy, bracing, and supportive care; steroids or emerging gene therapies for certain dystrophies.
Seizure and Epilepsy Disorders: Electrical Instability
Epilepsy is a neurological disorder defined by two or more unprovoked seizures. A seizure is a sudden, transient surge of abnormal electrical activity in the brain that causes involuntary changes in movement, behavior, or consciousness. Epilepsy is one of the most common reasons a child is referred to a pediatric neurologist.
- Types and Symptoms of Seizures
Seizures are classified by where they begin in the brain (focal or generalized) and how the child is affected.
- Generalized Onset Seizures (affecting both hemispheres):
- Tonic-Clonic (Grand Mal): The most recognizable type. Symptoms include sudden loss of consciousness, body stiffening (tonic phase), and rhythmic jerking of the limbs (clonic phase).
- Absence Seizures (Petit Mal): Characterized by brief, sudden lapses of awareness or staring spells, often lasting only a few seconds. The child is unaware during the episode and quickly returns to normal activity. These can be mistaken for daydreaming or ADHD inattention.
- Myoclonic Seizures: Sudden, quick, shock-like jerks of the arms, legs, or trunk.
- Focal Onset Seizures (starting in one hemisphere):
- Focal Aware Seizures (previously Simple Partial): The child remains conscious and may experience motor symptoms (jerking in one limb), sensory symptoms (strange smells, tastes, or tingling), or emotional symptoms (sudden fear).
- Focal Impaired Awareness Seizures (previously Complex Partial): Consciousness is impaired. The child may exhibit automatisms (lip-smacking, repetitive movements, fumbling with clothes) and appear to be in a trance or dream-like state.
- Diagnosis and Specialized Treatment
- Diagnosis relies heavily on clinical history and the Electroencephalogram (EEG), which records the brain’s electrical patterns. MRI is used to check for structural causes (tumors, stroke, malformations). Treatment involves Anti-Epileptic Drugs (AEDs), the Ketogenic Diet, or surgical intervention for specific types of refractory epilepsy.
- Acquired, Structural, and Infectious Conditions
These conditions result from trauma, infection, vascular events, or congenital abnormalities in brain structure.
- Traumatic and Vascular Conditions
- Traumatic Brain Injury (TBI) and Concussion: Damage caused by external force. Symptoms depend on severity but often include headache, nausea, dizziness, vomiting, confusion, and difficulty with concentration or memory.
- Pediatric Stroke: Occurs when blood flow to the brain is interrupted (ischemic) or when a blood vessel ruptures (hemorrhagic). Though often missed, it is a significant cause of motor and cognitive deficits.
- Symptoms: Sudden weakness or numbness on one side of the body (hemiparesis), slurred speech, or acute loss of balance.
- Infectious and Inflammatory Disorders
- Meningitis/Encephalitis: Serious infections causing inflammation of the membranes (meningitis) or the brain tissue (encephalitis).
- Symptoms: High fever, severe headache, neck stiffness, light sensitivity, and altered mental status. These require immediate medical intervention due to the risk of permanent neurological damage, including seizures and developmental regression.
- Multiple Sclerosis (MS) and Autoimmune Encephalitis: Conditions where the immune system mistakenly attacks the myelin sheath (MS) or brain proteins (Autoimmune Encephalitis). Symptoms can include acute weakness, vision loss, or rapid changes in behavior and cognition.
- Congenital and Structural Defects
- Hydrocephalus: The accumulation of excess Cerebrospinal Fluid (CSF) in the brain’s ventricles, causing pressure. Treatment often involves implanting a ventriculoperitoneal shunt to drain the fluid.
- Neural Tube Defects (e.g., Spina Bifida): Birth defects where the neural tube—which forms the early brain and spinal cord—does not close completely during fetal development. Symptoms involve varying degrees of lower limb weakness, paralysis, and bowel/bladder dysfunction.
- The Mandate for Holistic and Specialized Care
Given the complexity and interconnectedness of the developing nervous system, management of pediatric neurological disorders cannot be compartmentalized. It demands a specialized, holistic approach.
The experience of practitioners like Dr. Habib G Pathan, who manages complex conditions including epilepsy, febrile seizures, strokes, learning difficulties (dyslexia, dysgraphia), muscle disorders, developmental delays, ADHD, Autism, and Cerebral Palsy, underscores the need for a systematic and integrated approach.
At centers like the Dr. Habib’s Foster CDC, the goal is not merely to treat a single symptom, but to:
- Diagnose Completely: Use advanced tools (EEG, specialized neuro-imaging, and detailed developmental assessments) to identify the specific nature and extent of the disorder.
- Integrate Therapies: Coordinate a multidisciplinary team—including occupational therapists (OT), speech and language therapists (SLP), and behavioral therapists—to address all domains affected by the disorder.
- Empower the Family: Provide counseling and education to parents, transforming them into active participants in the child’s tailored, outcome-oriented care plan.
By focusing on a personalized, interdisciplinary strategy that targets both the neurological origin and the resulting functional impairments, specialized pediatric neurologists help children with these complex conditions maximize their capabilities and integrate fully into society.
FAQ
- Slow talk or real problem?
If a child is much slower than others in talking or learning, it may be a Developmental Delay. Conditions like Autism explain why this happens. See a doctor early. - Do seizures always mean Epilepsy?
No. One seizure can happen due to fever. Epilepsy is diagnosed only when seizures happen again without a clear cause. - First step if I suspect ADHD or Autism?
Visit your pediatrician or a Pediatric Neurologist and share what you observe. Early check-up helps start treatment sooner. - Why is Early Intervention important at Dr. Habib’s clinic?
Because young brains learn faster. Early therapy helps children improve and grow better. - Does Dr. Habib treat only walking problems?
No. He treats many conditions like Autism, ADHD, Epilepsy, Cerebral Palsy, and other brain-related issues in children.
Conclusion
-
The landscape of pediatric neurological disorders is vast and can feel daunting to parents. However, science has demonstrated that early diagnosis and timely intervention are not just helpful, but critical for fully harnessing the neuroplasticity of the child’s developing brain. Conditions like Epilepsy, Cerebral Palsy, Autism, and ADHD do not define a child’s potential; they only define the starting point of the therapeutic journey.
A holistic and multidisciplinary approach, guided by a specialist like a pediatric neurologist, is essential. This approach does not stop at symptom management but focuses on empowering the child’s innate abilities and providing a supportive environment that fosters positive growth and behavioral development. Every step forward, no matter how small, is a victory in a child’s developmental path. The ultimate goal, supported by specialized centers such as the Dr. Habib’s Foster CDC, is to ensure that children with special needs can thrive, participate fully in life, and reach their maximum potential.



Recent Comments